Sinus issues can be incredibly disruptive to your daily life. One common yet lesser-known condition is a “sinus shift.” This term might sound unusual, but it’s essential to understand what it means, its symptoms, causes, and how to find effective relief. In this article, we’ll break it all down into simple terms so you can take charge of your sinus health.
What is a sinus shift?
A sinus shift refers to changes in the position, pressure, or alignment of the sinus cavities. While not a medical term per se, it’s often used to describe the feeling of imbalance or blockage in your sinuses. This sensation can arise from structural issues, inflammation, or fluid buildup, leading to discomfort and potential health problems if left untreated.
Common symptoms of a sinus shift
The symptoms of a sinus shift can overlap with other sinus-related conditions. Recognizing the symptoms promptly can help you resolve the problem effectively. Here are some common symptoms:
- Facial Pain or pressure: Discomfort around your forehead, cheeks, or nose is a hallmark of sinus problems.
- Nasal congestion: Persistent stuffiness in one or both nostrils.
- Headaches: Especially those that worsen when bending forward.
- Post-nasal drip: A feeling of mucus dripping down the back of your throat.
- Dizziness or imbalance: A shift in sinus pressure can sometimes cause vertigo-like symptoms.
- Difficulty breathing: Blocked sinuses make it harder to breathe through the nose.
- Altered sense of smell or taste: Swelling or blockage in the sinuses can dull your senses.
If you experience these symptoms persistently, it’s time to take action.
Causes of a sinus shift
Several factors can contribute to a sinus shift. Understanding the root cause can help you pick the appropriate treatment. Here are some common culprits:
- Sinusitis: Both acute and chronic sinus infections can lead to inflammation and pressure changes.
- Allergies: Seasonal or environmental allergies can cause swelling and mucus buildup.
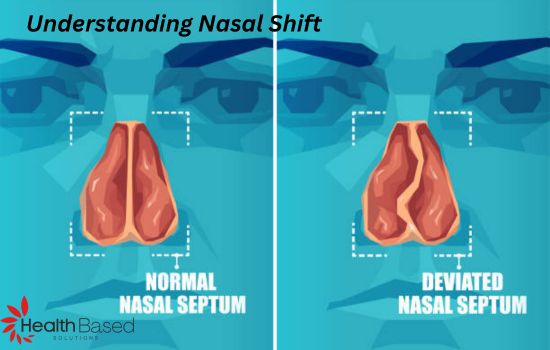
- Deviated septum: A crooked nasal septum can disrupt airflow and lead to pressure imbalances.
- Nasal polyps: These growths in the nasal passages can block the sinuses.
- Barometric pressure changes: Sudden changes in altitude or weather can affect sinus pressure.
- Infections: Viral, bacterial, or fungal infections can trigger sinus shifts.
- Trauma: Injury to the face or nose may lead to structural shifts in the sinuses.
Diagnosing
If you suspect a sinus shift, a visit to a healthcare professional is a good idea. Here’s what you can expect during the diagnostic procedure:
- Medical history: Your doctor will ask about your symptoms, duration, and potential triggers.
- Physical examination: Using a nasal endoscope, your doctor may check for blockages, swelling, or abnormalities.
- Imaging tests: X-rays, CT scans, or MRIs can provide detailed views of your sinus cavities.
- Allergy testing: Identifying allergens can help pinpoint the cause of chronic sinus issues.
Effective treatments for sinus shift
The good news is that a sinus shift can often be managed with a combination of home remedies, medical treatments, and preventive measures. Let’s explore these options in detail.
1. Home remedies
- Steam Inhalation: Breathing in steam can loosen mucus and reduce inflammation.
- Saline Nasal Spray: Keeps nasal passages moist and helps flush out irritants.
- Warm Compress: Using a warm cloth to your face can ease sinus pressure.
- Hydration: Drinking plenty of fluids facilitates thin mucus and promotes drainage.
- Rest: Giving your body time to recover is essential for any healing process.
2. Over-the-counter medications
- Decongestants: Temporary relief from nasal congestion. Use sparingly to avoid rebound congestion.
- Antihistamines: Effective for sinus shifts triggered by allergies.
- Pain relievers: Address headaches and facial pain associated with sinus pressure.
3. Medical interventions
- Prescription medications: Your doctor may recommend antibiotics if a bacterial infection is present.
- Nasal corticosteroids: Minimize inflammation and improve airflow.
- Allergy immunotherapy: Long-term solution for allergy-related sinus issues.
- Surgery: For severe cases, procedures like septoplasty, balloon sinuplasty, or polyp removal may be necessary.
Preventing sinus shifts
Prevention is always better than cure. By incorporating these habits into your daily routine, you can reduce the likelihood of experiencing a sinus shift:
- Maintain good hygiene: Regular handwashing can prevent infections.
- Use a humidifier: Keeping indoor air moist helps prevent nasal dryness.
- Avoid allergens: Identify and minimize exposure to allergy triggers.
- Stay hydrated: Drinking water keeps mucus thin and prevents blockages.
- Quit smoking: Tobacco smoke irritates nasal passages and can worsen sinus problems.
- Manage stress: High stress levels can weaken your immune system, making you prone to sinus issues.
- Exercise regularly: Physical activity boosts circulation and helps clear nasal passages.
When to see a doctor
While many sinus issues resolve with home care, certain situations call for professional help. Seek medical attention if you experience:
- Persistent symptoms lasting over 10 days.
- Severe facial pain or swelling.
- High fever along with sinus symptoms.
- Vision changes or eye pain.
- Recurring sinus infections.
Note: Prompt intervention can prevent complications and ensure effective treatment.
Conclusion
Sinus shifts can be uncomfortable, but understanding their causes, symptoms, and treatments can empower you to take control of your health. Whether through home remedies, medications, or preventive measures, relief is within reach. If symptoms persist, don’t waste your time to consult a healthcare provider. With the accurate approach, you can breathe easier.
Start implementing these tips today and give your sinuses the care they deserve!